Understanding Herniated Discs: Causes, Symptoms, and Treatment Options
Imagine waking up one day with a persistent pain radiating through your back and down your legs, putting a halt to your daily activities. This is a reality for many suffering from a herniated disc, a common yet often misunderstood condition. A herniated disc, also known as a slipped or ruptured disc, occurs when the soft cushion between the bones in your spine pushes out, potentially pressing on nearby nerves. This article will delve into the intricacies of herniated discs, including their causes and symptoms, various treatment options, and tips for prevention. Additionally, we will discuss real-world examples and statistical data to illustrate the prevalence and impact of this condition on individuals. By the end of this piece, you’ll be equipped with valuable insights to understand and manage herniated discs effectively.
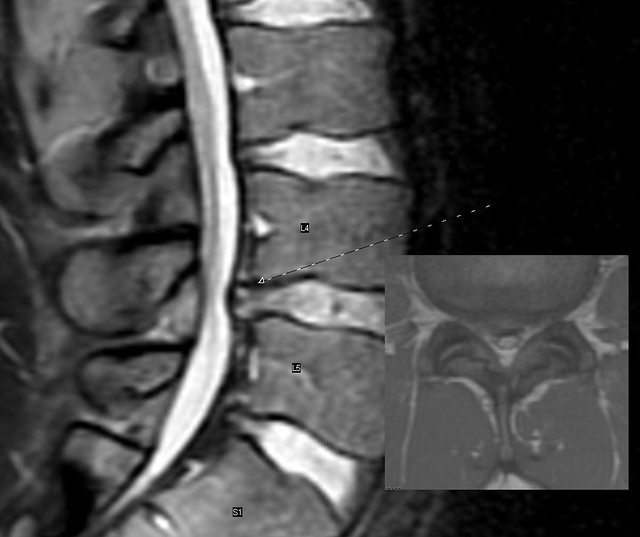
What is a Herniated Disc?
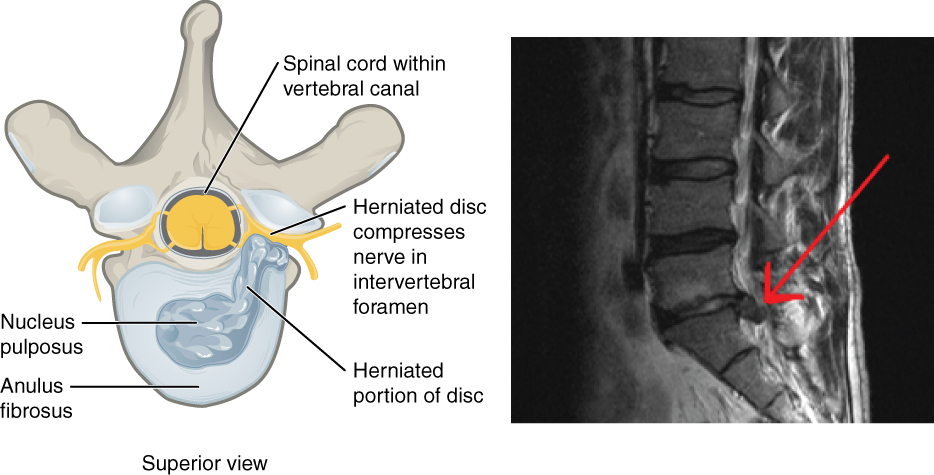
A herniated disc occurs when the inner gel-like material of a spinal disc, known as the nucleus pulposus, protrudes through a tear in the outer layer, called the annulus fibrosus. This condition usually happens in the lumbar or cervical region of the spine. Herniated discs can be caused by a variety of factors, including age-related degeneration, injury, or repetitive stress on the spine. According to the American Academy of Orthopaedic Surgeons, approximately 1-2% of the population experiences a herniated disc at some point in their lives. Notably, herniated discs are often asymptomatic, meaning many individuals may not realize they have one until they undergo imaging for other conditions. However, when symptoms arise, they can include severe pain, numbness, tingling, and weakness in the arms or legs. Understanding the anatomy of the spine and the mechanics behind disc herniation is crucial to grasp the severity and implications of this condition.
Symptoms of a Herniated Disc
The symptoms of a herniated disc can vary widely, depending on the location of the herniation and the extent to which it affects nearby nerves. Commonly, individuals may experience localized pain, which can be sharp or dull and may worsen with certain movements. For instance, a lumbar herniated disc can lead to sciatica, where pain radiates from the lower back down the legs, often described as a burning or electric shock-like sensation. It’s estimated that about 90% of those with a herniated disc can have radiating pain, which reflects nerve involvement. In contrast, cervical herniations may cause symptoms in the neck, shoulders, and arms, potentially resulting in weakness or coordination difficulties. According to recent studies, nearly 30% of patients with a herniated disc report chronic pain lasting longer than 6 months, underscoring the substantial impact on quality of life. Recognizing these symptoms early on is vital for obtaining a timely diagnosis and initiating appropriate treatment.
Diagnosis of Herniated Discs
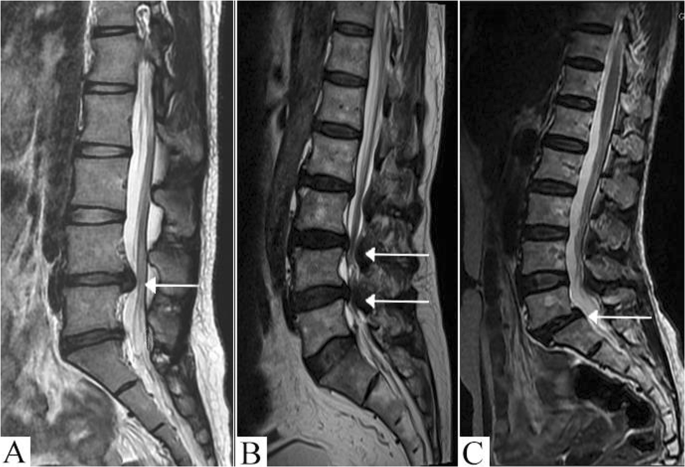
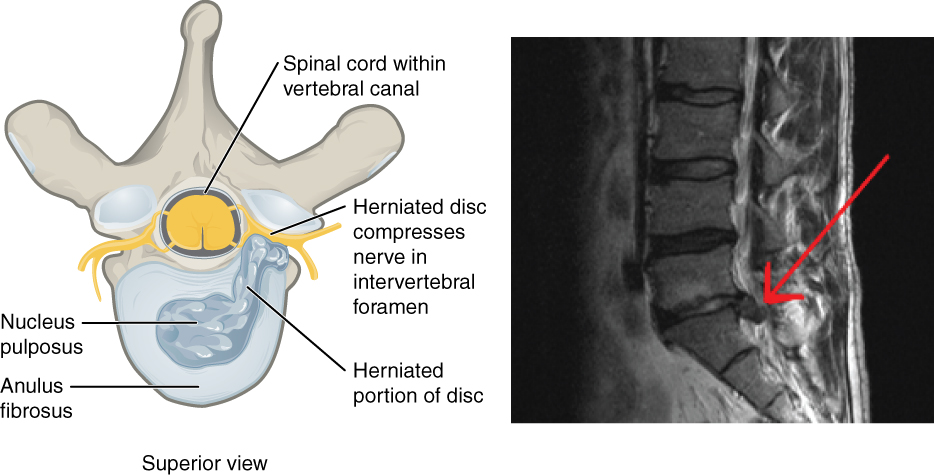
Diagnosing a herniated disc typically involves a combination of physical examinations, imaging tests, and patient history. Healthcare providers will often begin with a comprehensive physical exam, assessing the range of motion, reflexes, and areas of tenderness. Following this, imaging techniques such as X-rays, MRIs, or CT scans may be utilized to visualize the spine and identify any disc protrusions. In some cases, doctors may also use electromyography (EMG) to assess nerve function. Research indicates that MRIs are particularly effective in diagnosing herniated discs, with an accuracy rate of over 90%. It’s important to understand that while imaging can pinpoint the presence of a herniated disc, it does not always correlate with the severity of symptoms. Many individuals with herniated discs lead active lives without requiring surgical intervention, emphasizing the need for a personalized approach to diagnosis and treatment.
Treatment Options for Herniated Discs
Treatment for a herniated disc varies based on symptom severity and individual patient needs. Initially, conservative treatments, such as rest, physical therapy, and medications (including NSAIDs), are recommended for managing pain and inflammation. Studies show that approximately 80-90% of patients improve with non-surgical options within a few weeks to months. Physical therapy may involve exercises designed to strengthen the spine and improve flexibility. In more severe cases, or if conservative treatments fail to provide relief, surgical options may be considered. The most common surgical procedure is a discectomy, where the herniated portion of the disc is removed. According to the American Academy of Orthopaedic Surgeons, about 5-10% of patients with herniated discs undergo surgery. Post-surgery, patients often participate in rehabilitation programs to facilitate recovery and prevent recurrence. Overall, it’s critical to work closely with healthcare professionals to determine the best course of action for each unique situation.
Preventing Herniated Discs
Prevention of herniated discs largely revolves around maintaining a healthy lifestyle and practicing good body mechanics. Engaging in regular exercise strengthens the muscles that support the spine, reducing the risk of injury. Activities such as swimming, walking, and strength training are particularly beneficial. Furthermore, maintaining a healthy weight can alleviate unnecessary strain on the spine, as excess weight can increase the likelihood of disc degeneration. Proper lifting techniques, such as bending at the knees instead of the waist, can also minimize the risk of injury. According to the National Institute of Neurological Disorders and Stroke, making these adjustments can significantly reduce the incidence of herniated discs. Education about the importance of ergonomics in the workplace, such as using chairs that support the lower back, plays a crucial role in prevention. By adopting these strategies, individuals can greatly enhance their spinal health and decrease the likelihood of experiencing a herniated disc.
In summary, a herniated disc can be a debilitating condition, but with proper understanding and management, individuals can navigate the challenges it presents. Key takeaways include recognizing the symptoms early, understanding the diagnostic process, and exploring a range of treatment options from conservative to surgical. As we have seen, prevention is equally important, and adopting a healthy lifestyle can significantly lower the risk of developing a herniated disc. If you or someone you know is experiencing symptoms associated with this condition, it’s vital to seek professional medical advice. Don’t let a herniated disc dictate your life; take proactive steps towards treatment and prevention. For more information or support regarding herniated discs, consult a healthcare professional or visit reputable medical websites to stay informed and empowered.